Faces And Stories Of People With Mental Or Physical Illnesses: 16 Portraits I Took
Since my mid-twenties I had been dealing with something that did not make sense to me and I felt that no one would understand. I carried my loneliness and it became heavier and heavier the more I kept it to myself. One day, I stumbled upon somebody else’s story. I read her story and through her words, I saw myself. That gave me hope and I realized the power of sharing our stories.
After losing someone I admired to suicide in 2018, I decided to create “A Part of Me” project. Using my photography skills, I capture each person’s raw emotions while interviewing them. I then use my storytelling skills to write their stories and send them to my editor Adi Ferrara. Once the stories are ready they are published alongside the person’s portrait photo.
I worked on the project for three months prior to the launching in January 2019 and I publish a story every Tuesday at 8 a.m. (NZ time). This important project comes as a second job for me and I hope to make it my full-time job.
To support the project, please head over to my Patreon page.
More info: patreon.com | Facebook
Robert – Post-Natal Depression
When Robert’s partner got pregnant he was overjoyed. He had known he wanted to be a dad ever since he was 14. When his son was born the experience was everything he thought it would be. He was there for the birth, he was there to catch his newborn son, and he was there to cut the umbilical cord. It was exactly how he imagined the moment of birth to be.
Things soon changed for Robert, and not for the better. He began to feel numb and empty, and this wasn’t at all the reality of fatherhood that he’d expected. As more people were invited into the young family’s life to meet their newborn son, he felt his relationship with the baby change and break down. He felt constantly numb.
To make matters worse, while Robert’s relationship with his partner was good and healthy at the time they conceived, during the pregnancy Robert’s partner suffered from constant morning sickness. As her condition started to affect her daily functioning, resolving issues that came up in their relationship wasn’t possible. As a result, Robert and his partner broke up only three months after their son was born.
Robert moved out, found a good job and was earning good money and visited his son weekly. However, without knowing what was happening to him, his lifestyle deteriorated along with his mental health. He lived on pizza, smokes, and booze. He was drinking heavily every moment he could and went from visiting his son every week to only seeing him fortnightly. Though the change in visits routine was partly due to his work schedule, Robert says it was more so because he just didn’t feel that he needed to see his boy. He no longer felt connected to his child. His feelings revolved around a sense of obligation to the baby, not actual love.
A lot of us associate depression with isolating one’s self and pushing people away, but in Robert’s case, he was using human interaction and alcohol to mask what was happening in his head. If he was surrounded by people, he didn’t have to think. If he had enough alcohol in his system, he couldn’t think. He self-medicated with alcohol in order to stop his mental anguish from consuming him completely.
The first thing Robert did coming home after work was to go and have a drink. He would constantly invite people over, in order to not be left alone with his thoughts. This went on until the day he decided to have his drink after smoking. He walked outside to smoke, and a tidal wave of emotions hit him. He crashed.
Robert sat on the deck for hours, consumed by his own thoughts, feeling that he failed his family, friends, and son. During those hours of anguish, as he failed to respond to messages and calls, some of his friends became concerned. One of them came to Robert’s place, and even though Robert’s flatmates said he wasn’t home, this friend simply knew Robert was home. He went around the house to the deck and found Robert holding a knife to his throat. After the initial shock and a long conversation, Robert’s friend got him to drop the knife and took him to the hospital.
They waited roughly three hours, during which Robert tried to leave six times. They were finally seen by someone in the psychiatric ward. That was when Robert was diagnosed with post-natal depression.
Like many men before him, Robert argued that he’s a male and therefore cannot suffer from post-natal depression. The psychiatrist repeated his diagnosis and told Robert that about ten percent of men suffer from it. Most of them go undiagnosed. The psychiatrist also assured Robert he’s going to get through it. Despite Robert’s blunt assertion that he was going to finish what he started on the deck if he was released, he was discharged from the hospital. Luckily, his friend didn’t leave his side until Robert was no longer a danger to himself.
Robert is now in a much better place. He and his son Slade share a very close relationship. He understands the disconnected feeling from his son was due to his post-natal depression. He is helping others who are having a hard time by managing the Facebook page Suicide Awareness / Prevention and talks publicly about male post-natal depression to raise awareness of the condition.
Cherie – Premenstrual Dysphoric Disorder
Throughout the years Cherie could not understand why her periods were so painful; doubling over in pain, feeling heavy and feeling exhausted all the time was all just part of her life. But while she always had difficult periods, when she was 33, things got worse. Leading up to her periods would be 2 weeks of misery — she would be constantly exhausted and angry, snapping at everyone. Looking for answers, Cherie went to a doctor specializing in women’s health and explained her symptoms. The doctor ordered some scans and tests. When the results came back the doctor dismissed her worries and told her, “you are fine, you are just getting older.” Being only 33 years old at the time, his assertion did not sound right to Cherie. She was frustrated by the doctor’s diagnosis but went home and tried to deal with it all, not knowing she was actually suffering from Premenstrual Dysphoric Disorder (PMDD).
Over time, unfortunately, things only got worse. Cherie was constantly exhausted, and the pain affecting her bladder and bowels got so bad at times that she feared she won’t be able to control her body for the amount of time needed to drive if she went out. She was also almost always grumpy, as the pain took a heavy emotional toll on her.
And then anger reared its head. Cherie managed to mostly keep her anger under control at work but at home would find herself lashing out at her husband and son, whom she felt were “the worst people in the world” at the time. At this point she had almost no break from her symptoms; after her period would end there would be a few days of peace before the cycle would start all over again.
When she was 37, Cherie could not take her physical and mental anguish anymore and went to see her doctor. She shared with the doctor both the physical symptoms alongside the homicidal and suicidal thoughts she had been having. That was when Cherie learned her condition had a name and an explanation. “It is basically PMS on steroids”, she says. While a person without the disorder might get two or three days of period pain and experience some emotional effects, with PMDD you get 2-3 weeks of it. “It is like being two people,” she adds, “you have one week where you are absolutely fine and then the two weeks leading to your period you have got all sorts of things you are dealing with.”
Cherie received Depo Provera injections to stop her periods and was put on antidepressants. The antidepressants helped with most of the anger symptoms, and she found that knowing she had PMDD helped her realize that her reactions might be coming from her condition. This knowledge helps her cope with the anger by taking a step back, going for a walk, or otherwise distracting herself before acting on her emotions. With her new treatment and some support from international support groups that she joined, Cherie feels like a new person. She is active again and able to take part in things she neglected because of her condition.
“If you fear you might suffer from Premenstrual Dysphoric Disorder and didn’t get diagnosed yet, remember that your feelings are valid,” she says, “and don’t stop until you find a doctor that actually knows it is a real thing and will figure out how to help you.”
Pitena – Depression
When Pitena was a teenager she felt “things weren’t right” with her, but at the time she was just put on vitamin b and no further action was taken. Depression and mental health in adolescents weren’t really issues that were considered or discussed. It wasn’t until her early twenties that she was finally put on antidepressants, but at that time her depression was classified as situational depression. She lost her six-days-old daughter not long before diagnosis, and told the doctors she was depressed and upset. They gave her pills to deal with the pain but offered no additional support, such as counseling.
A little later that year Pitena decided she needed a fresh start and moved to Christchurch, where she and her doctor started on a journey to find the right medication for her. It wasn’t easy but eventually, they did find a medication that worked and she felt very lucky. Unfortunately, the medication she was on was defunded by the government 10 years later, and so her pharmacist changed Pitena’s medication to a generic one. Within six months of the change, without her realizing it, her condition worsened.
“I was on the street with my girlfriend,” she recalls, “and she was telling me I was losing it.” As the change was gradual Pitena was unaware of how bad things got, but that conversation opened her eyes. Pitena then went to her doctor, who explained the differences between left and right brain pathways of depression. She realized the problem was the generic medication does not specify which depression pathway it is meant for. “It made life a little easier,” she says, “knowing that it wasn’t me actually getting worse, it was the medication.” With her doctor’s help, they then found the right medication for her once again, and she was fine for a long while.
When Pitena was 35, three years after they found the right medicine for her, she started feeling ill. She went to the doctor and found out she was pregnant again. Instead of enjoying her pregnancy, the emotions from her previous pregnancy and the loss of her baby resurfaced, and for the first time, she grieved the loss of her daughter. Alongside these difficult emotions, while dealing with a number of other personal matters, Pitena also had to decide whether she will stay on her antidepressant medication during the pregnancy. With her doctor’s help, Pitena decided to reduce her medication’s dosage. “Every day I was just trying to get through, trying to survive,” she says. Though difficult at the time, Pitena got through the pregnancy and now has a healthy 16-years-old son.
After years of being stable on her medication, changes brought on by menopause when Pitena was in her 40s meant that her trusted regimen was no longer working. She once again embarked on a journey to find the right medication, with guidance and support from her doctor. Despite a false start she managed to get back on track fairly quickly. “It took me a long time to realize I am never going to be off medications,” she says, “It is a hard thing to admit, but the medication is not changing who I am, it’s just tuning out the imbalance to allow me to actually be who I really am.”
“Trying to explain depression to people and how we end up breaking down from something as small as stubbing our toe, I use the snowflake analogy,” she explains, “Every day every person gets a snowflake, hundreds of snowflakes. You break your nail on the table, you missed the bus, you are busy at work — every little thing is a snowflake. And they may build up a little bit into a snowball at times but on a normal day, those snowflakes melt. When you suffer from depression sometimes those snowflakes just do not melt, they are just accumulating. Suddenly there is this huge mountain, all created by snowflakes and you just stubbed your toe and there is an avalanche coming down on you and you just collapse from the weight of a mountain of snowflakes. And it is important to remember that it is ok to cry, it is ok to take some time to self-care.”
Jessie – Depression and Anxiety
Ever since Jessie was born she was an anxious child. Her parents had lovingly called tending to her needs “Jessie duty.” When she was a young teenager, Jessie would react to things differently than her friends, in a more melodramatic way, but for her, it was just normal behavior. Looking back, Jessie recalls crying, getting upset and offended a lot. She now feels she was taking things to heart more than she should have.
As a teenager, Jessie was rather clever, but her anxiety often took over, making her feel she wasn’t smart enough or good enough and would never reach her full potential. These thoughts and feelings created a vicious cycle that kept her from actually reaching her full potential. At the time Jessie was young and did not yet realize that she was living with anxiety and depression. Her parents, unaware of her condition, did not know how to help her either. Looking back Jessie feels she needed more support than most teenagers normally do. She needed the people around her to remind her of her worth. Mostly she wishes there was more awareness and less stigma surrounding the issue of mental illness, so she could have asked for and gotten the help she needed in time.
Jessie’s anxiety worsened during her teens. She started to recognize what she thought were societal standards — things you should or shouldn’t do, things to wear in order to be “cool” and the pressure of deciding her future. Jessie fluctuated between not caring what others think, wearing whatever she liked, and feeling awesome and confident, to fearing that because she was so different people would judge her harshly. When Jessie was 16, her anxiety got to the point where she experienced an attack around her hair not sitting the right way on her head. She felt ugly and stupid and ended up shaving her head. That moment of panic and that anxiety-driven decision lingered with her as people continued asking why she did it. She remembers having to hide tears of embarrassment about her baffling condition.
The big wake-up call came on mufti day at school. Jessie tried on the clothes she chose for herself, but when she looked in the mirror she felt dumb. Her anxiety took over and her thoughts swirled over what other people are going to think of her. She ended up having an anxiety attack. Seeing her daughter’s distress, Jessie’s mother allowed her to stay home from school. Later on that same day, Jessie’s mother realized she did not see Jessie for a while and went looking for her. She found Jessie in her bedroom in the nick of time — the girl had overdosed on her mother’s heart medication.
At first, Jessie was devastated that her suicide attempt failed. She spent a few days in the hospital and was referred to a child psychologist. The time following her suicide attempt wasn’t easy; Jessie was dealing with difficult emotions. She felt like a burden and a failure, and still wanted to finish what she started — killing herself. But despite the difficulties, things were looking up because Jessie was finally able to get the support she needed. Along with her psychologist, her family, and her friends, Jessie was able to learn ways of coping with her illness that still serve her, and will continue to do so for the rest of her life.
For the longest time, Jessie hated thinking about her suicide attempt. “It is hard enough for a parent to lose a child to a car accident or any sort of natural cause,” she says, “but to find out your child tried to do that to themselves is really gut-wrenching.” Now, Jessie loves the bond she shares with her mother. She is happy to be here ten years later and be able to talk openly about her feelings in a way that does not hurt either of them —they both know she is sharing her story to help others. As a redo for her 16-year-old self, Jessie shaved her head again, but this time for a good cause – she was fundraising for the Mental Health Foundation.
“Depression might convince you that the world is better off without you, and I know you are hurting,” she says, “but there are so many people that love you and can help you get through, because no one wants to live without you.” “I hope one day you will truly be happy and live well with your mental illness,” she adds, “It may take time, but you deserve it and with the right love and support I promise it’s worth it.”
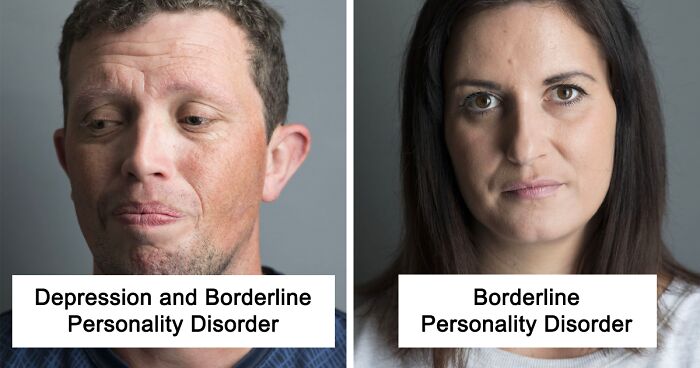
Nadia – Borderline Personality Disorder
Nadia found out she has borderline personality disorder when she was in her early 20s, but her story starts long before that. When she was 9-years-old Nadia was sexually abused. She kept this incident a secret for many years but started to act out. That same year she made her first suicide attempt. In truth, however, she felt different long before she was 9, as she was always unable to regulate her emotions like the other kids.
“Borderline personality disorder is often caused by childhood trauma,” she says. “We are not horrible people and are not out to hurt people.” Growing up Nadia didn’t have a stable childhood and her needs were not met. She felt insecure as a child, a feeling that stayed with her when she grew older and affected her in many ways. Her grandparents eventually took her in, providing the stability she needed, but by that time she was a very angry child. At age 15 she started cutting herself.
Nadia has three older children. She would have loved to be more present in her children’s lives but lost custody of them due to her mental illness. People sometimes say to her “when you get better,” hoping that one day she will “snap out of it” not understanding that her disorder is a lifelong one.
Nadia makes sure she is completely honest when dating someone new, but she finds that the less they know the more they like her, which puts her in a difficult position. Her potential partners often say “it’s too much for me to deal with”, “When people don’t understand it makes it more difficult, it hurts to not be understood,” she says.
Borderline personality disorder is different from one person to another, but as Nadia describes it, people with the disorder experience emotions much more intensely than what an “average person” would feel. “When I’m happy,” she says, “I feel euphoric.” She has the tendency to fall in love and get attached very fast and her mood is a little like a roller-coaster and can go between different emotions fairly fast. She finds it difficult to maintain a healthy relationship and tends to overthink situations. When people are upset with her, her disorder causes her to jump to the conclusion that they hate her, instead of understanding that they are just upset with something specific she did or said. It leads her to end relationships as a defense mechanism to prevent the other person from leaving. Alternatively, she finds herself trying to commit suicide or engaging in self-harm when all she wants is for them to care — she simply doesn’t know a healthy way to ask.
During a bipolar episode, Nadia feels like she’s not herself and is unreachable and cannot be comforted. With the help of medications and therapy, she has reached a point where she can see the warning signs of an impending episode and regulate her emotions better, but the struggle will always be there.
Hannah – Anxiety
Looking back, Hannah was always an anxious child. She always likes being in control and would repeat things over and over again until they were perfect. She recalls acting this way since she was about 10, and remembers getting extremely frustrated when things weren’t perfect. This continued in high school, where Hannah struggled with exams but still managed to be a straight-A student. But she was anxious just going to school in the morning. Her way of dealing with it at the time was to wake up 2-3 hours before she had to leave the house, in order to feel like she was in control and able to ease into the day. At that point, even though there was a history of mental illness in Hannah’s family, she did not think she was living with a mental illness — she always managed to keep her anxiety under control.
Hannah continued to use her anxiety control methods in university as well, but when she started working in the corporate world it became a problem —she did not have as much control over her life anymore. Eventually, with added responsibilities and deadlines closing in, she became overwhelmed and was unable to function in her role. She found herself crying on her way to work, dreading another day of overwhelming tasks and expectations she could not live up to, in her mind.
To make things worse, she was also in a relationship that was not good for her. When the relationship started falling apart, Hannah was unable to function. In a way, dealing with the aftermath of the breakup was the easy part, as difficult and dreadful as that part was. As long as Hannah had something to focus on – for example, dealing with legal matters in the wake of the breakup – she was able to keep on going. But after the battle ended, everything crumbled. It was when she couldn’t perform even the most basic activities, such as sending an email or cooking a meal, that she realized she had a problem.
Hannah’s anxiety took over. “It makes you almost numb,” she says, “because you are thinking of so many things at once, all the time, you cannot focus on one thing.” She wasn’t sleeping or eating, she stopped going to the gym and going out with her friends, and from the moment she woke up she felt she was having “mini heart attacks”. Hannah had that feeling in her chest for weeks at a time and got to the point where she was unsure whether this feeling was ever going to go away. While Hannah’s friends and family were very supportive, she still found it difficult to reach out, as she is always the one who takes care of everyone else and sorts things out. She did not like asking for help. She has since gotten better at asking, but it has been a learning curve.
With Hannah’s success at work, most people would not imagine that she is actually living with anxiety and takes medication to cope with it. She can function well at work but can still have meltdowns about things like clogged sinks or packing a suitcase. “When you have anxiety the most ridiculous things can throw you off the edge,” she says. “Having a mental illness is not a failure or lack of you as a person, it is a long term condition that goes up and down and can actually rear its head for no particular reason — it is just in you.”
She reflects that even though everything feels really hard at times, it is really important to look for the right support. Hannah has tried different ways of coping and realized that she needs medication and support to keep balance. She finds that the most helpful ways of dealing with her anxiety have been talking to a counselor to learn coping skills, and doing physical activities. She likes walking her dog in nature and lifting weights in the gym to help her unwind. She also finds journaling and listening to podcasts useful, and makes room in her schedule to just do nothing at all.
David – Traumatic Brain Injury
In April 2008 David was out having a few drinks with a co-worker. It seemed like any other night out and they were chatting with a guy on the street when everything changed. David doesn’t remember what he said to the guy, but that person sure did not like what David said. One punch to the jaw was all it took. David fell backward and cracked his head on the concrete.
“The first thing that I remember was waking up in my own bed,” he recalls, “sore jaw and sore back of my head, blood and fluid all over.” He did not remember how he got to his bed, nor did he remember why his head was bleeding. It wasn’t until a few years later that David discovered what actually happened that night. He chose not to press charges against the man who assaulted him.
After waking up David went to see a doctor who took one look at him and called an ambulance. David was rushed to the hospital and ended up spending the night there. The doctor said David was lucky to be alive and not be a paraplegic. He suffered a traumatic brain injury (TBI), and there was a three-inch fracture at the base of his skull.
Following the diagnosis, David had a month off work, but after his time off ended he was forced to go back. Despite the fact that he didn’t feel ready. After going back to work David was constantly exhausted, sleeping at least 12 hours each day. Commuting took about an hour and a half of his day and he would work 8 hours a day. By the end of a workday, David was left with about two and a half free hours. “I wasn’t living, I was just existing,” he says.
A lot has changed after the assault and David struggled with things that weren’t a challenge for him before. Among other things, it became difficult for David to understand big words and he could only read a few paragraphs before getting too tired. He lost his sense of smell, experienced headaches and migraines, became sensitive to sound and light, and his long and short term memory were affected.
After the 2011 earthquake in Christchurch, David was made redundant at work and given severance pay. “It was the best thing for me,” he says, “I was really struggling with things but was too scared to leave.”
David feels very let down by being forced back into work after the assault and is trying to go through his Accident Compensation Corporation (ACC) file to build up a case, but he is still struggling. Since reading is difficult for him and the medical jargon requires him to do a lot of research the case just drains him. “It’s just like a tap,” he says, “you might as well just turn on my energy and watch it flow out.”
David found that people around him didn’t understand the changes he was going through because his injury was (and still is) invisible. “If someone was to have a car accident and lose the use of their legs, then you can see that they are in a wheelchair, they can’t use their legs and you can understand, ‘oh, I get it, this changed you, you’re in a wheelchair, I understand why you’re so frustrated because you can’t walk anymore’, where it’s internal and invisible people don’t tend to look at you the same way.”
David is now at peace with what happened. His attacker apologized and David forgave him. Looking back, though, he was angry, he says: “I was angry not only at him but angry around a lot of things because it changed me, I became somebody else and that was really frustrating, to try and adapt to all that change was quite hard. I went through a lot of different emotions over a lot of months, trying to deal with everything. I am always learning about myself and trying to find ways to improve things and make things easier.”
After the assault, David picked up photography and music promotion as a hobby and he is now working on becoming a motivational and educational speaker about TBI. “It’s all well and good having all these doctors and specialists that have all these degrees, but it’s not the same when you actually hear it from somebody who actually lives it,” he says. “The brain is such an amazing organ that I fully believe that even if you were to have two people with absolutely identical injuries the results would be different.”
Naenae – Epilepsy
When Naenae was 20, two people she knew pushed their way into her home and started beating her, following a previous dispute. Naenae tried to fight but fell to the ground and endured several kicks to her head before passing out. When she came to she was alone. She made her way outside, screaming for help, and walked towards a neighbor’s door. She remembers hearing them talk to police before passing out on their doorstep.
A few months after the attack Naenae started having unexplained symptoms that included fainting or instances when her entire body would shake. Unsure of what was happening she consulted her doctor. She was diagnosed with post-traumatic stress disorder and her symptoms were classified as panic attacks. “I listened to my doctor and took the pills he gave me,” she says, “they made me feel better about the fact I was having the attacks, but it was still happening.” She went back to her doctor and was put on more medication. After the change in medication Naenae ended up having a full-blown seizure in front of a friend who was familiar with epilepsy and he encouraged her to go see another doctor.
Naenae went back to her doctor and when she brought up the option of epilepsy he dismissed it. With the support of her friend Naenae went to see another doctor and was indeed diagnosed with epilepsy, a year after the attack. The new treatment didn’t stop the seizures entirely, but it lengthened the time between the seizures, and reduced their severity. Her epilepsy seemed to be a progressive disease, and Naenae had to change medications from time to time when the old ones stopped working as well as they used to. She would often have an aura before a seizure, which allows her to get herself to a safe place before the seizure started. Depending on how comfortable she felt with the people around her and how severe she thought the seizure is going to be, Naenae would sometimes alert someone so they can help.
When she was 26 Naenae’s epilepsy was diagnosed as refractory, which means the medications were not working for her anymore. As the body’s general wellbeing affects the probability of a seizure, Naenae started trying to make sure her life was well balanced with regards to food, sleep, stress levels and other lifestyle choices she could control. When she was 31 Naenae found neurofeedback treatments, and discovered that listening to music when the aura starts really helps her.
While she is unable to work, Naenae volunteers as much as she can. “Wherever anybody needs me I just go,” she says. She volunteers with cosplayers at fairs, feeds the homeless, helps coordinate events, and helps with the Suicide Awareness / Prevention Facebook page. “I probably live a fuller life because of my illnesses,” she says, “I probably wouldn’t live the same way or be the same person if it wasn’t for how sick I actually am.” Naenae used to wear boys’ clothes as she was worried about being exposed if she had a seizure, but things are different now. She started dressing up as a doll in the beginning of 2018 and it makes her extremely happy. “I have realized how short Life can be,” she says, “if I have a seizure in a dress I have a seizure in a dress. It doesn’t worry me as it did before.”
“Every single person is different with their epilepsy, but also every seizure can be different,” she says. “There are seizures that look bad and mean nothing and you can still get up and function, while there are good seizures that look like you are ok but do you over for days. It’s not what’s going on on the outside and people can see, it’s what’s going on inside your brain.”
Selina – PTSD, Anxiety and Depression
Selina’s upbringing wasn’t the happy childhood you’d wish upon a child. There was emotional and physical abuse in the family, and her father took his own life when she was only four. Selina herself endured sexual abuse for three tormenting years, starting when she was 10. “I felt that I had to do what he wanted me to do, or else I would get in trouble,” she recalls, “I was scared and thought I was doing something wrong.”
After over three years of living with sexual abuse, at the age of 13, Selina shared her secret with her sister, who informed the authorities. She was taken to the police station to give a statement and her abuser was eventually jailed. She was also removed from her home by social workers and placed in a foster home. While her foster parents were a welcome change from her unhappy home environment, other members of the foster family were a little harder for Selina to cope with. Selina’s cousin, seeing how unhappy Selina was, applied for custody of Selina. After a year living with the foster family, Selina moved to her cousin’s custody, staying there until she was 18.
During her early teen years, Selina would only express happiness. She remembers feeling numb and using happiness to mask what her real emotions were. Looking back, she can see early signs of her post-traumatic stress disorder (PTSD), but at the time she was obviously unaware of what she was experiencing.
Selina started going to counseling when she was 18. Her counselor helped her through reliving some of the difficult memories she blocked until then. The therapy allowed her to confront her past and her emotions, rather than blocking them. “I was never into sex as a teenager,” she says, “it scared the hell out of me to even get close to people.” It wasn’t until Selina was 25, after being with her then-partner for five years, that she was able to face her fears and be more intimate. “Some people just don’t understand what it means to have sexual related PTSD, most people just associate having PTSD with soldiers and the war,” she says, “so a lot of people live with it without even realizing that.”
When Selina was 26, the February 2011 earthquake struck Christchurch and retriggered her symptoms. She was finally diagnosed with PTSD, depression, and anxiety and put on antidepressants for 9 months. She is unsure as to why her counselor didn’t diagnose her when she was 18, but thinks they might have been cautious not to overwhelm her at the time. Selina can now appreciate her ex-partner and friends for their understanding, and believes their support was very important for her progress. “Finding people that understand and went through similar things helps a lot,” she says. “With the #MeToo movement a lot more people come forward that wouldn’t come forward before.”
Looking back Selina wishes she’d reached out and gotten help and counseling sooner. She still has triggers that provoke a resurgence of her symptoms, and sometimes she gets overwhelmed, but Selina is in a much better place overall. She is surrounded by supportive friends and family members and is in a loving and caring relationship. She practices self-care by gaming, reading, writing, and talking to people, all of which help her cope with her emotions. “I try to slow down and look after myself,” she says, “just take a break from everything else.”
Ethan – PTSD and IBS
Ethan remembers being bullied from the time he was 5. He was always laughed at for being overweight and was excluded from events. When he was 9, Ethan went to overnight camp with his school. He was very excited when a few boys and a girl he liked invited him to hang out at their cabin. Everyone was laughing and things seemed to be going well for a change. But then one of the boys started laughing at Ethan, calling him fat and demanding that Ethan takes off his shirt. Ethan refused and in return, the boy pulled a knife and threatened him. Scared and alone in front of a crowd of bullies Ethan complied and then ran out of the cabin, crying. He spent the rest of his time at camp hiding. He was forever changed by these events, but kept them a secret and started slipping into depression. He started distancing himself from everyone and the stress he was experiencing pushed him into unhealthy eating habits trying to cope with his escalating emotions.
The bullying didn’t stop. Ethan was bullied by both students and teachers throughout the years. At times he tried reaching out for help within the school. But even when one of the teachers physically assaulted him, the school authorities didn’t do anything. Feeling hopeless, Ethan then confided in his mother about the bullying at school. “She was very sympathetic, but lost on what to do,” he says. Not wanting to burden his mother further, Ethan kept his fears to himself and his worst memory — the camp incident — was still a secret.
Feeling terrified and defenseless Ethan’s depression got worse and he started self-harming. He also tried to commit suicide several times. After his first suicide attempt, Ethan was sent to counseling and was diagnosed with depression. “I didn’t have any friends, I didn’t want any friends,” he says, “I didn’t want anyone to feel my burden.” Yet trying to deal with his emotions on his own was overwhelming. At times Ethan wanted to reach out but was too scared to do so, and his stress-eating got worse.
When Ethan was 17 he started experiencing a lot of abdominal pain and was worried that he might have appendicitis. “It feels like something sharp is stabbing me in the gut,” he describes. After six months of tests, Ethan was finally diagnosed with Irritable bowel syndrome (IBS). Since being diagnosed Ethan has tried numerous treatments but nothing seems to release the condition’s grip on his life. “Sometimes I’ll be too sore to go out, or I’ll be so bummed out that I wouldn’t want to go to work,” he says, “because I’m too sore to move.”
The trauma caused by the camp incident affected Ethan tremendously. “I can’t go on buses because I’m terrified, I can’t go near schools because I freak out,” he says, “and it’s hard for me to make new friends and open up to people.” But Ethan never gave up. When he was 18 Ethan joined a youth group. He started developing his social skills and was able to form a relationship with one of the boys. Since then Ethan has worked hard and is now in a better place. He is writing music and is learning to do ring announcements and interviews for wrestling events. “It will help me get the tools to be able to overcome that fear, that’s what I’m hoping,” he says. Ethan knows now that his friends love and support him, and is able to share his story in hopes of easing the loneliness and fears of others.
Wendy – Fibromyalgia
At age 24 Wendy was experiencing soreness and fatigue that wouldn’t go away. She went to see a doctor, who ordered blood tests. The results came back showing high ANA antibodies count, and Wendy was told she might get osteoarthritis when she was older. No treatment was prescribed and Wendy was still sore and tired. However, she did not pursue the issue until almost a decade later.
When Wendy was 33 she noticed a sharp pain in her big toe and went to see a doctor again. Blood tests once again showed high ANA antibodies count, but also showed Wendy was pregnant. Her symptoms were yet again not addressed, and during her pregnancy, Wendy’s condition started deteriorating. At the time, Wendy was running her own business as a sports massage therapist and it became very difficult for her to work. “I was going into work and I couldn’t straighten my hands out, and then I’d start massaging with my forearms instead,” she says.
Wendy ended up losing her baby. She got pregnant for the second time and lost her baby again and then got pregnant for the third time and had a stillbirth. Her condition continued to deteriorate, “I couldn’t get out of bed and slowly my movements started to shrink back and back and then I became sort of stuck in bed,” she recalls. She sold her business and stayed in bed for months. At age 34 she and her first husband adopted their son. “When I first got him I couldn’t move my body, it was really painful and I used to change his nappy using my wrist and I’d be sitting on the floor playing with him fine one minute and go get up off the floor and I couldn’t stand up.” Her husband at the time did not understand what she was going through and she felt very lonely.
When her son was 3 months old, Wendy was wrongfully diagnosed with polyarthritis and among other medications, she was put on Celebrex. The treatment helped Wendy feel better and start working again but she later discovered the terrible impact it had on her health.
When her son was 13 months old Wendy’s marriage ended. She was still treated for polyarthritis and that helped her cope but the constant pain was always there. “I feel like someone has a voodoo doll shoving hot needles into my bones and into my joints,” she says. Wendy felt very lonely; she was an adoptive mom but was still grieving the loss of her biological children and her failed marriage. “I was completely abandoned and no one understood that I was just trying to survive my day just by breathing,” she says.
It wasn’t until Wendy was 43 that she was finally diagnosed with fibromyalgia. Wendy also met her childhood sweetheart around that time and they fell in love again and raised her son together. When the family was struggling financially, and Wendy’s son asked for music lessons, she decided to go back to practicing massage therapy from home so they can afford the lessons for him. She worked for a while until she was diagnosed with pulmonary embolism when she was 45, the result of her Celebrex treatments. “I was told by doctors ‘you’ll never massage again, you won’t work again’ that’s what put me to bed,” she says, “You believe what the doctors say.”
Wendy spent months in the hospital. She was taken off the treatment for polyarthritis and her symptoms grew worse. “I ended up in a wheelchair, unable to move. I couldn’t even hold a cup to my mouth to have a drink of coffee,” she says, “ my family had to put straws together and I had to drink sucking up through a straw.”
When she was 48 Wendy decided to make a change. She was lying in bed alone one day while her husband was at work. The pain was unbearable and wishing it all to end she went back to sleep as that was the only time she was free from the pain. “I remember thinking to myself when I woke up the next morning, ‘lie here and die in agony or get up feel your agony but make some memories’,” she says, “and that’s what got me moving.” She set up a massage bed in her home and started booking clients. It was a long process, but every day Wendy managed to do a little more.
Wendy is now successfully running her sport massage business and finds that a low salicylates diet helps with her pain. She still wakes up sore and stiff, but has learned to manage the pain.
Hunter – Suicide Attempt and Addiction
When Hunter was 10 his parents separated for a while. He was staying with his father at his grandmother’s house when he woke up one day and couldn’t shake the feeling his mother was in trouble. “The way I explain it is I could hear my mom screaming from the depth of hell,” he says. Hunter then woke up his father and urged him to go home to check on his mother. When Hunter and his father arrived at Hunter’s childhood home they found the house locked up and his mother passed out in the garage — she had attempted suicide. Hunter then ran to the neighbors and they called an ambulance. When the ambulance got to the scene the EMT told Hunter that if they were just a few minutes later his mother would have died.
Two weeks later while Hunter was staying with his mother and some friends of hers, Hunter was passing by the bathroom when all of a sudden he had a feeling his mother was there and was in trouble again. He told his mother’s friends that he thinks she’s in there and they broke through the door to find Hunter’s mother. She had attempted to commit suicide again and was found not a moment too soon.
Seeing his mother in such horrific situations really affected Hunter and he carried the trauma with him. Hunter was struggling to cope and became a very troubled boy. At age 14 he was admitted to the acute psychiatric ward at Princess Margaret Hospital for a couple of months, and following his release continued going to counseling.
Despite the counseling, Hunter was still struggling to cope with his pain. A few family members introduced Hunter to marijuana when he was 15. “I felt like I had found something,” he says, “Something that really gave me courage, something that let me eat, something that helped me sleep.” Hunter became addicted to the drug and would do almost anything to get it. He was consumed by his addiction. When he was 26 he was introduced to methamphetamine. Two years later Hunter’s addictions included methamphetamine and alcohol as well.
Throughout the years Hunter attempted to end his life several times and had trouble maintaining relationships. He has four children from four different partners. “I always struggled in relationships because I hadn’t found myself,” he says, “so I couldn’t offer anybody love and I couldn’t give my kids love because I didn’t love myself.”
When Hunter was 30 he started losing touch with reality, as a result of his meth use. “I am God, I have the answers that you need, I am the one who will restart and save the world,” he recalls telling people. He was admitted to Hillmorton Hospital for psychosis. During his time in Hillmorton Hospital Hunter started using his music as a tool of healing. To this day Hunter really appreciates Hillmorton Hospital for letting him have his music equipment in his room and feels it was the key to his recovery.
Hunter always had a special connection to music and after his release from Hillmorton Hospital became an independent artist in New Zealand. He is now producing music and merchandise with the help of his mother. “Music saved my life and now I want to use music to save other people’s lives,” he says.
Hunter is now working hard to stay in recovery. Unfortunately, he never met his youngest daughter, due to his history of substance abuse. “All I can do is be a better me so when she comes I will be the father that she needs,” he says. Hunter lives with his mother who fought her own battle with addiction. “Our thoughts are our reality and our reality are [sic] our thoughts,” he says, “it’s like two wolves that live inside us, and they are fighting every day and the one that we feed the most is going to win so I feed the good wolf.”
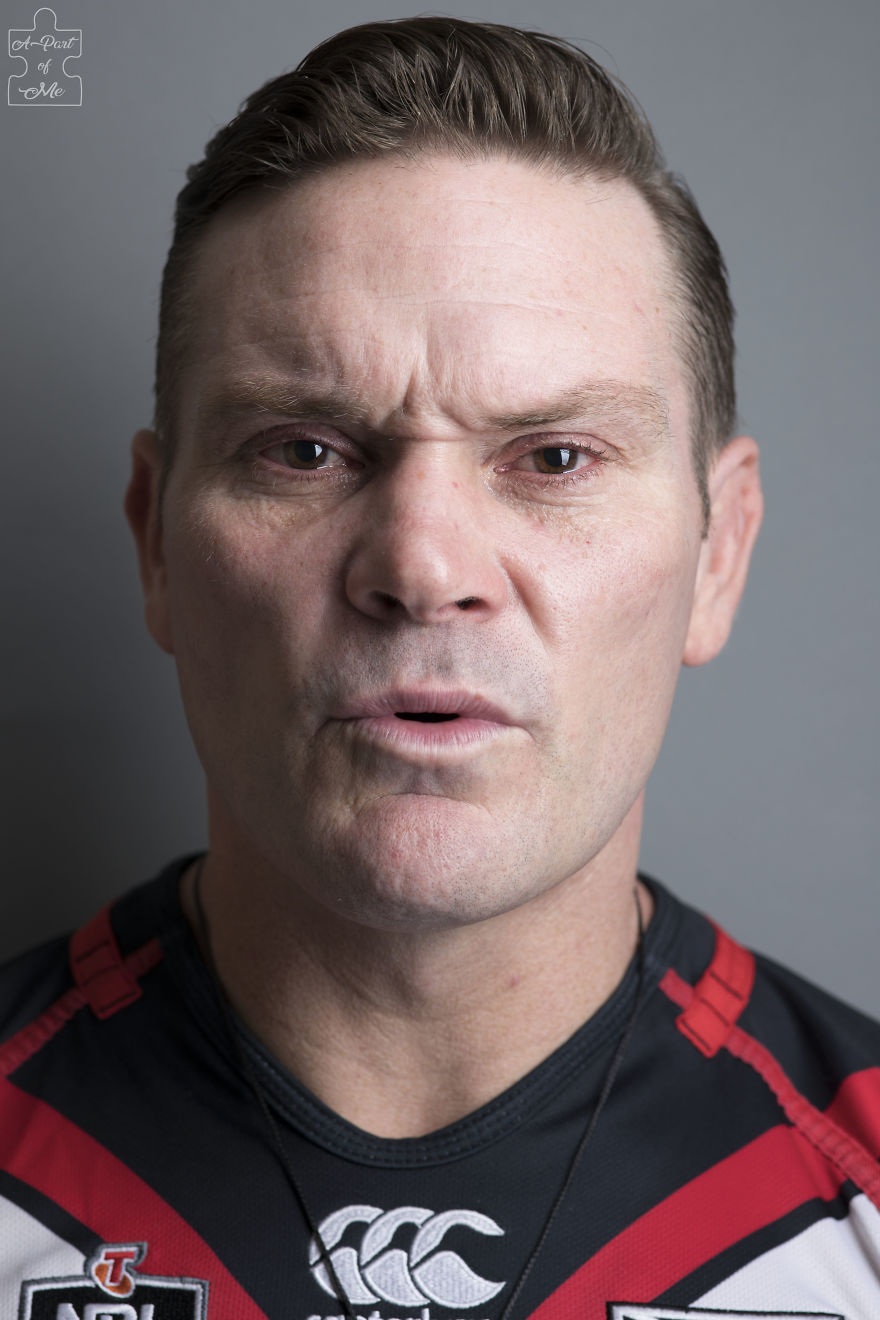
Scott – Anxiety, Panic Disorder and Depression
Scott remembers having learning difficulties since he was eight years old. Even though his family made an effort to look for answers, the results were inconclusive. The struggles and difficulties carried through the years and the older he got the harder it was for him. “As a kid individuals pick up your struggles and I got picked on a lot,” he says. He was always a sensitive person and would often get bullied for that.
The bullying died down after Scott moved schools when he was 16. As a sixth former, Scott was still struggling with his studies and was put with the fifth formers. “It was quite embarrassing,” he says, “I felt quite uncomfortable, felt out of place.” But things changed the moment Scott’s new teacher, Mr. Smith, walked through the door. It was Mr. Smith’s flamboyant personality and unique approach that captivated Scott so much and for the first time, Scott was engaged in his studies.
Seeing Mr. Smith laughing off the remarks thrown at him was eye-opening for Scott. “Back then being a homosexual was a huge thing, and this man wasn’t just homosexual, he was a teacher!” he says, “I admire [sic] this man.” Scott’s attitude changed completely. He looked forward to going to class and enjoyed learning. Seeing the change in her son Scott’s mother supported him with after-school English lessons. Within half a year Scott was number one in his English class and couldn’t be prouder.
By the end of the school year, Scott was finally able to pass his exam. “I have failed every single written exam just because of my anxiety,” he says, “I still hadn’t been diagnosed back then but I was extremely anxious.” Every time Scott had an exam he would experience shakes, cold and hot sweats and mental blocks causing him to completely shut down. Even though Mr. Smith was told by other teachers Scott was a lost cause, he never gave up on him and that meant the world to Scott.
From school, Scott went straight into the workforce. A few years later when Scott was 21, he was experiencing severe anxiety that made it extremely difficult to function at work and in his daily life. Scott was told he had a mental illness and was put on Cepramil, an anti-anxiety medication, for the first time, but wasn’t thoroughly examined or given a diagnosis. “Before that, I didn’t know I had a mental Illness,” he says, “I just didn’t feel right.”
Throughout the years Scott changed medications and dosages when needed but was not given a proper treatment to help him develop the tools he needed to cope with his complicated mental illness. “It would work for a wee while but then I’d fall back, I can’t explain, you blame yourself,” he says, “You ask yourself sometimes why aren’t I getting better? Or why aren’t I improving? Why am I going two steps forward and like five or six steps backward? Why? Why do I think this way?” With so many questions left unanswered, Scott was trying to control his life to the best of his ability.
When Scott was 36 his grandfather passed away after a battle with cancer. Dealing with the loss of his grandfather alongside an unhealthy environment in his workplace brought Scott to a breaking point and he had a meltdown at work. Scott’s fellow employees tried to comfort him but when they failed they arranged for him to be taken home. Following the incident, Scott’s wife took him to the doctor. He was advised to take time off at work. He was put on benefits for a few months but ended up staying off work for a whole year. Looking back Scott doesn’t think that was the right decision for him or his family.
When Scott chose to go back to work it wasn’t easy but with his wife’s support, he was able to find the strength he needed. “She is my best friend, she is my rock,” he says, “I wouldn’t have got to where I am today without her support in the background.”
In 2018 when Scott was 42 he was finally referred to a psychologist and got his diagnosis. After living with anxiety disorder, panic disorder, and depression for most of his life, now he had answers. “When I heard that, I felt a little bit of weight lifted off my shoulders,” he says. Since then Scott has learned different coping tactics and finds mindfulness really helps him.
“I was considered a guy that can take care of himself, a guy that had it all going on but inside I was a desperate, at time helpless, struggling human being,” he says, “mental illness does not discriminate, mental illness doesn’t pick and choose who it goes for – it takes everybody. But how you deal with that and what you do with it is the key.”
Jeremy – Depression and Borderline Personality Disorder
When Jeremy was 18 his then partner discovered she was pregnant. Being religious, they decided to “do the right thing” and get married. “I think the shock of having a first child at the age of 18 and also being married was quite a big thing in life,” he says, “especially being so young.” At first, everyone was excited and everything was good, but when Jeremy left his job to become a stay-at-home-dad, things took a turn for the worse. Jeremy was struggling and started self-harming.
A couple of years later Jeremy’s wife was pregnant with their second child and things were still very hard for him. Jeremy was in and out of work, continued self-harming, and attempted to end his life a few times. This affected Jeremy’s relationship with his wife tremendously, and put their children at risk of being taken away. “Some people even saw it as a ticking time bomb,” he says.
Even though Jeremy was very grateful for his wife’s support he had trouble expressing himself and his emotions. After 7 years of being together, they decided to end their marriage. “Things went a lot further downhill from there, trying to understand that I am now about to go through a divorce at the age of 25,” he says, “I had everything I wanted in life and now that’s gone.”
When Jeremy tried to reach out to people in his community he felt that his emotions were not addressed and that he was expected to just “get over it.” Even his close family struggled to understand what he was going through and the way he was dealing with it. “To me, a lot of the time, self-harm was a huge thing,” he says, “at the time it made me feel better but looking back at the scares and the hurt that I have done it got me thinking.” Unsure of whether he’s doing the right thing by asking for help, or even talking to the right people, Jeremy took a hard look at his life. He put on a fake smile and stopped talking to people about his pain, but deep down he was hurting so much he just wanted it all to end.
Four years after the divorce, while Jeremy was still struggling, his father was admitted to the hospital with heart problems. Jeremy made sure to spend every possible moment by his father’s side and did not leave the hospital even when his father went into what was supposed to be a four-hour surgery. After 11.5 torturous hours, one of the surgeons came out and told Jeremy that his father was not going to survive. “I didn’t really know what to do,” he says. As his father’s next of keen, Jeremy was asked to make the difficult decision of discontinuing life support.
After his father’s passing Jeremy was in a very bad place, “I was so far down I actually didn’t care about my life,” he says. Jeremy attempted to commit suicide repeatedly. “Everyone were worried, they had no idea what I was going to do next and at this stage, I fully broke down.” Jeremy looked at himself and didn’t recognize the person in front of him, “something needs to happen and it needs to happen now,” he recalls thinking.
Jeremy then found the strength to reach out for help. He messaged the Facebook page HopeWalk Christchurch, and for the first time, his mother was informed (by the page administrator) of the full extent of what he was going through. “She turned around and said she’ll do whatever it takes to get me the help that I need,” he says, “and I didn’t think she would.” But she did.
With his mother’s support, Jeremy was finally able to face what happened in the hospital. “Things are just too much,” he recalls telling her, “when I said to turn dad’s machines off, to me it felt like I killed my dad, and I couldn’t forgive myself.” Since then Jeremy, unfortunately, had a fall out with his mother, but he has made some great changes in his life. He has a full-time job that he loves, his relationships with his friends are flourishing. He has recently been diagnosed with borderline personality disorder in addition to his depression and started on a new medication that seems to work well for him. “Now I know while having depression and all this other stuff, I can reach out,” he says. “I know that there are so many people there for me, that are willing to support me in whatever way I need.”
Therese – Suicide Attempts and Addiction
Therese is the youngest of six sisters and grew up around substance abuse. When she was 14 family members introduced her to alcohol and drugs. She then started experimenting and her addiction progressed to include more drugs.
When Therese was 16 she met her children’s father. “He was a musician and he was in a band called The Androids and he was a bit older than me,” she says. The group was very much into alcohol, drugs and partying and for three years Therese was a part of their scene. She got pregnant when she was 19 and decided to stay clear of alcohol but kept on smoking marijuana.
After Therese gave birth to her daughter she went back to her old habits over time. She then followed one of her sisters, who struggled with substance abuse as well and decided to go to Queen Mary Hospital. Therese went to an alcohol and drug program and for the next 16 years, she was clean.
During that time Therese’s relationship with her husband wasn’t stable and he would break up with her and then come back quite often. The two had their second child and became practicing Christians for 9 years. Therese tried her hardest to fit in and be a good Christian wife and mother but felt out of place. “I would go to these prayer groups with these other ladies who were more [sic] older than I was,” she says, “and I would get them to pray for me because I didn’t believe that I was good enough for God to hear my prayer.”
Looking back Therese recalls a teacher calling her dumb in school and that stuck with her. She remembers feeling she wasn’t a good enough throughout her childhood and the feeling followed her into motherhood as well. “I was a very emotionally distant – shut down; I didn’t know how to connect with my kids, didn’t know how to play,” she says, “I missed out on a lot.”
By the time Therese was 33 she was struggling with her emotions but unaware that her mood was deteriorating. A stressful event in her life that she didn’t know how to manage left her feeling her family would be better off without her. “People find it really hard to understand, talking about suicide being selfish and to them it is,” she says, “but to myself [sic] it was like I was being selfish by staying alive and causing them all the pain and the misery that was happening.”
Therese didn’t know who to turn to; she was suffering and felt that the easiest way out was to not be on this earth anymore. After two weeks of planning, Therese attempted to end her life while her son was staying at his grandmother’s house with her husband. In the middle of the night, her son woke up worried about her and urged his father to head over to her home. She was found unconscious by the two and was rushed to the hospital. “You would hope that when someone came out of that they would be so grateful that they were alive,” she says, “I wasn’t. I was so so angry.”
Therese’s family tried to support her but she was still suffering on her own. She attempted suicide again and her mother gave her an ultimatum. Therese would either voluntarily commit herself to Sunnyside Hospital or she would be forcibly committed. At that point, Therese knew her mother was right and chose to enter the mental hospital voluntarily. She stayed in the hospital for two weeks and made a pact with herself that suicide is never going to be an option again.
When Therese was 36, then sober for 16 years, she broke up with her husband permanently. In a simple act of celebration, she relapsed. For three years afterwards, Therese was drinking heavily. It wasn’t until she nearly died from alcohol poisoning that she decided to give up drinking again.
Therese has been sober for the past 17 years. She found that art therapy helps her deal with her emotions. She got her degree in Alcohol and Drugs Studies and has been working in the Alcohol and Drugs and Mental Health fields. Therese feels that as a recovering addict she has a responsibility to share her story, and as a suicide survivor she the responsibility to show that suicide doesn’t have to be an option. Therese is working with her son towards helping others with their struggles. They are both part of the King Cass Movement and encourages others to share their story. “Nothing we do can stop someone from killing themselves if they want to do it,” she says, “but we can give someone hope and might be able to reach a person.”
Bernice – Dissociative Identity Disorder
From the time she was 4, Bernice was sexually, physically, and emotionally abused by a family friend. Her parents were unaware of what their daughter was going through. Since the start of the abuse Bernice was experiencing blackouts, but it wasn’t until she was 12 years old and that she realized that’s what was happening.
Throughout her childhood and teenage years, Bernice’s home life was also tumultuous, and difficult for her to handle. At 16 she decided to move to Christchurch with her then-partner. After the move, Bernice started drinking and taking drugs to cope with her real-life nightmares.
A year after the move, Bernice got pregnant. Her partner ended the relationship while she was 5 months pregnant with their daughter. With no money and far from her family, her ex-partner’s family took her in and treated her as a daughter. It was while living with her ex-partner’s family that Bernice met her current husband, Bruce. At the time, neither one of them realized that she had been living with dissociative identity disorder.
By the time her daughter was born Bernice was very ill, “I was dissociating all the time, I couldn’t take care of her or myself,” she says. “For a long time it scared the crap out of me, because for me it was just lost time. I didn’t know what was going on.” Bernice lost hours at a time and had no memory of what happened during that lost time. “One minute it’d been 2 o’clock in the afternoon and the next minute it would be 7 o’clock at night,” she says. “I didn’t know what had happened who was looking after my kid, what I was doing, how he [her husband] was dealing… nothing!” It wasn’t until much later that Bernice and Bruce learned that when their children were in danger, the Bernice personality was in charge.
Bernice and Bruce were struggling and were seeking help, but time and again psychiatrists had no answers. Bernice was finally diagnosed with dissociative identity disorder when she was 22, after almost two decades of living with it. It took another two years for the couple to find the right therapist for her. “In those days it was extremely rare, especially in this country,” she says. “When I was diagnosed, I was one of 3 in the country who have been diagnosed with dissociative identity disorder.” Up until the time she started therapy, Bernice’s personalities could only express themselves while she was blacking out. “It took 8.5 years of full-on therapy to get to a place where I could communicate with them, they could communicate with me, I could maintain some kind of control and manage them in a way that we learnt to live as a community,” she says.
Before the therapy, it was Bruce who communicated with the personalities and learned as much as possible about them. Bruce would ask the personalities questions and would sometimes even re-live the episodes that created them. “Each individual personality has its own reason for being here,” Bernice says. “It has its own birth from trauma, but it also has its own purpose.” Bruce joined Bernice’s therapy sessions, and was able to fill in the gaps and help both her and her therapist understand her situation better. “Any normal bloke would’ve bolted and thought ‘stuff this I am not putting up with this,” she says. “He’s not normal, he’s bullheaded and stubborn.”
Having dissociative identity disorder can be challenging but Bernice finds it also has a few perks. Living with 14 personalities allows Bernice to be a better problem solver. She also finds it easier to connect with her grandchildren, as one of her personalities is 4 years old. “My grandchildren are similar ages to Neessy now, so I am the fun one,” she says, “because I can see what they are trying to do, I understand their kind of play and on good days I can even let Neesy out to play with them.”
After learning so much during therapy, Bernice and Bruce are in a better place now. She is very grateful for Bruce’s support throughout the years and is working hard to help others and raise awareness around mental health. “Recovery can build the kind of person who everybody needs in their lives,” she says. “By building the resilience and the support networks and being able to share the knowledge and experiences that each and every person has, that makes society a better place.”
47Kviews
Share on FacebookIt's easy to forget, I think, that every person has a story. Sometimes we are so absorbed with ourselves that we don't pay attention to the person in front of us in the checkout line, or the guy who flipped us off for "no reason". I think that we need to remember that all those people - even the ones we dislike or even hate - have their only little stories. Every car that you pass by in the highway has a person in it that has some kind of pain. We all have a story. Just a thought.
I think I will continue to read your comment every morning for the rest of my life... Unfortunately I'm very bad at remembering this :/
Load More Replies...I actually made an account so I could comment on this. Thank you for sharing these people's stories. I am living with a few mental health conditions and it's hard. One of the things that helps is knowing you are not alone.
Trust me, you definitely aren't alone. I'm a mental hot mess.
Load More Replies...As a person living with BPD, I relate to Nadia's story intimately. The only difference between her story and mine is that my life (up until about 3 years ago) was peppered with self harm and suicidal tendencies. Thanks to therapies including CBT & DBT I have managed to turn my life around. I still struggle, and desperately want to harm (I think this is something I'll have to fight for the rest of my life), but I continue to revisit my DBT skills, re-do the coursework, and follow up regularly with my therapist. No drugs are needed with BPD, though some use them to treat coinciding illnesses such as anxiety and depression. Personally, I've never found a drug that helps more than self reflection, in the moment responses, and proper communication. BRAVO to everyone brave enough to show the real faces of mental illness! :D
Probably unlikely, but I wish I could ask you questions about your experiences
Load More Replies...It's easy to forget, I think, that every person has a story. Sometimes we are so absorbed with ourselves that we don't pay attention to the person in front of us in the checkout line, or the guy who flipped us off for "no reason". I think that we need to remember that all those people - even the ones we dislike or even hate - have their only little stories. Every car that you pass by in the highway has a person in it that has some kind of pain. We all have a story. Just a thought.
I think I will continue to read your comment every morning for the rest of my life... Unfortunately I'm very bad at remembering this :/
Load More Replies...I actually made an account so I could comment on this. Thank you for sharing these people's stories. I am living with a few mental health conditions and it's hard. One of the things that helps is knowing you are not alone.
Trust me, you definitely aren't alone. I'm a mental hot mess.
Load More Replies...As a person living with BPD, I relate to Nadia's story intimately. The only difference between her story and mine is that my life (up until about 3 years ago) was peppered with self harm and suicidal tendencies. Thanks to therapies including CBT & DBT I have managed to turn my life around. I still struggle, and desperately want to harm (I think this is something I'll have to fight for the rest of my life), but I continue to revisit my DBT skills, re-do the coursework, and follow up regularly with my therapist. No drugs are needed with BPD, though some use them to treat coinciding illnesses such as anxiety and depression. Personally, I've never found a drug that helps more than self reflection, in the moment responses, and proper communication. BRAVO to everyone brave enough to show the real faces of mental illness! :D
Probably unlikely, but I wish I could ask you questions about your experiences
Load More Replies...

















279
100